Star & HEDIS Quality Programs
What is our approach for enhancing quality?
At Magellan Rx Management, we are eager to roll up our sleeves and lean into the complex pharmacy challenges that are impacting our customers and members. We have been at the forefront of developing and implementing innovative clinical programs to help customers achieve and maintain up to 5-Stars and improve performance measures. Our dedicated leadership team consisting of doctors, pharmacists and clinicians stay ahead of existing and upcoming quality measures to improve our member’s overall care.
What our Star and HEDIS Quality Programs offer:
 Advanced analytics
Advanced analytics
Magellan Rx leverages pharmacy and/or medical claims data to identify baseline and recurring outreach opportunities
 Dynamic platform
Dynamic platform
Our clinical team utilizes a proprietary platform to track all interventions and generate detailed reporting including population and member-level metrics
 Clinical outreach
Clinical outreach
All outreach to members, prescribers, and pharmacies is conducted on behalf of the health plan utilizing plan-specific documents and information that summarizes the program, recommendations and clinical guidelines.
Programs such as:
- Statins in Persons with Diabetes
- Statins in Cardiovascular Disease
- Diabetes Medication Adherence
- RAS Antagonist Adherence (Hypertension)
- Statin Adherence (Cholesterol)
- Diabetic Care – Eye Exam
- MTM Program (Link to MTM page) Completion Rate for a CMR
- Osteoporosis Management
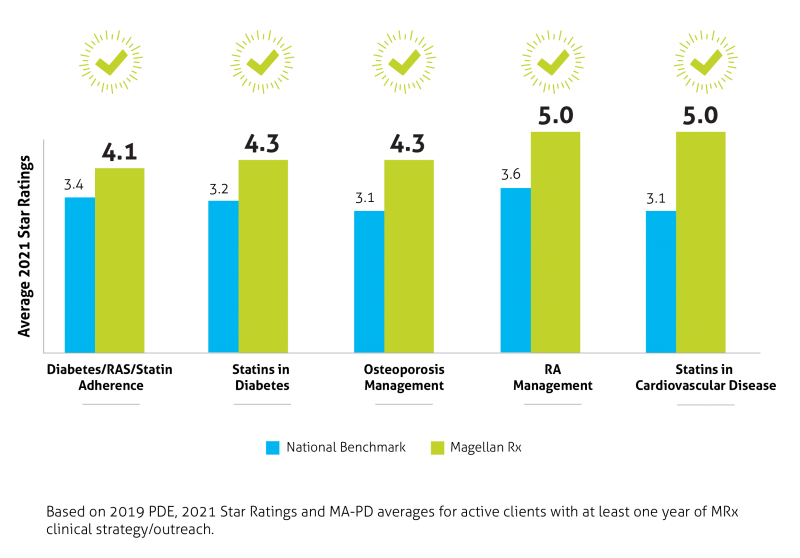
Results
Clinically we manage over one million lives across multiples lines of business for up to 18 health plans. Not only do we meet the national benchmark, we beat it! See for yourself!
Who can use our Star and HEDIS quality programs?
Our Stars and HEDIS quality programs are available to health plans, employer groups, and government entities, who are seeking data-driven, evidence-based, and personalized interventions to stay ahead of existing and upcoming quality measures and improve the health of their members. We closely monitor for all measures provided by CMS to ensure the best plan experience for Medicare beneficiaries.
Get more information
If you want to learn more about our Star and HEDIS clinical programs or have questions – contact us.